Covid-19 has exposed and exacerbated health inequalities in the UK. During this time, health inequalities have been discussed more frequently, as they are recognised as a serious problem that needs addressing. But it’s not always clear what exactly the problem is and what actions we can take to help. Young people’s health inequalities are rarely talked about. In this blog post, Rachael McKeown offers some clarity by providing our new definition of health inequalities that is specific to young people.
As we reflect on the impact of Covid-19, it is clear that the pandemic has had an unequal impact across the country. It was not the “great leveller”, as once mentioned, but rather the opposite. It has revealed the inequalities that exist in our society and our health. Young people have experienced huge upheavals during this period, with unprecedented changes to education, university, employment opportunities and their social lives when they were unable to see friends and family members in lockdown periods. Arguably, this generation of young people have taken a disproportionate hit from the pandemic. Within the age group, the experiences haven’t been equal as some young people have fared worse than others, particularly those from disadvantaged backgrounds or minority groups. As a result, we have seen a widening in the health inequalities experienced by young people.
So, what are these health inequalities and why do they matter to young people?
Most people point towards differences in life and healthy life expectancy to explain health inequalities, which shows that where you are born can have a major baring on the length of time that you are likely to live. But this measure does not feel as relevant when thinking about young people’s health inequalities. It can seem ‘far off’ for young people who are at the start of their transition into adult lives.
Yet we know that there differences in young people’s health now, in the present. A really clear example of this is the latest data on the number of 10-11 year olds in England who are overweight or obese. 33.8% of young people who live in the most deprived areas are classified as obese, compared to 14.3% of those in the least deprived areas. And there are a number of other health topics where we see similar trends in young people’s health.
But when we think about young people we also have to consider how their health status now influences their ability to form a solid foundation for a healthy future. Poor health and coping strategies developed in adolescence can lead to health conditions later in life. The health behaviours young people form and their ability to manage their own health conditions are crucial for determining their future health.
At AYPH, we hadn’t come across a definition of health inequalities that captured all of these difference aspects and made sense for young people. We are proposing using the following definition for young people’s health inequalities going forwards.
So, how are health inequalities in young people caused and what can we do about them?
Ultimately, health inequalities are caused by the economic inequalities in society. Access to financial resources allows young people to live healthy lives. Yet we know that child poverty rates are high and the number of secondary school pupils claiming Free School Meals has risen from 12.4% in 2018 to 18.9% in 2021.
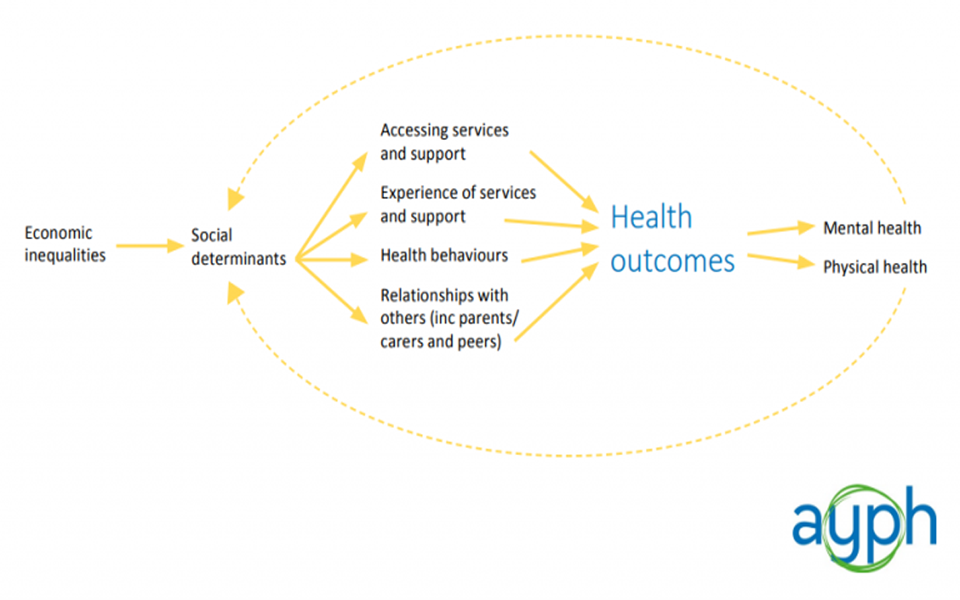
The “social determinants” of health have been called the “causes of the causes” of ill health. We have not come across a complete list of the “social determinants” of health that affect young people as they are complex, multiple and overlapping factors. However, we believe the following to be particularly relevant: education, employment, geography and the physical environment, housing, transport.
Our conceptual model for young people’s health inequalities:
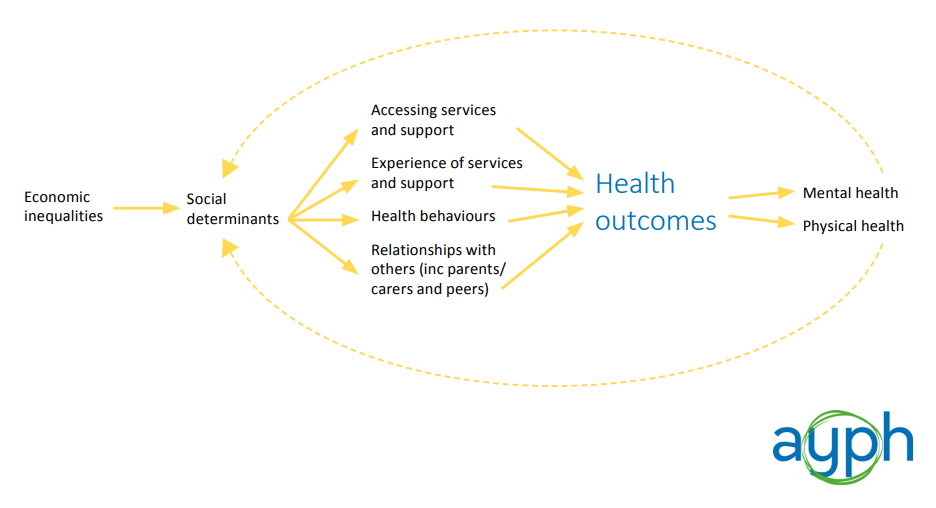
Importantly, we have identified an intermediary part of the model where the “social determinants” of young people’s health are translated into different health outcomes. We are calling these the “levers”, where young people are presented with either opportunities or barriers to achieving good health. These are:
- Accessing services and support
- Experiences of services and support
- Health behaviours
- Relationships with others (including professionals, parents / carers and peers)
We believe that these “levers” are a good place to start in terms of targeting interventions and resources to reduce young people’s health inequalities. It is important to keep in mind that the relationship in this conceptual model is by no means deterministic.
You can read more about the causes, drivers and outcomes of young people’s health inequalities in our new briefing paper ‘Clarifying what we mean by health inequalities for young people’.
This work contributes to our wider Health Inequalities Policy Programme, which is part of the Health Foundation’s Young people’s future health inquiry. If you would like to get involved or request to be kept in touch about this work, please contact us: rachael@youngpeopleshealth.org.uk